A case of pulmonary complication of sickle cells disease
C. Torregiani1, S. Tommassetti2, M. Confalonieri1, V. Poletti2
1 U/O Pneumologia Ospedale Cattinara Trieste Italy 2U/O Pneumologia Interventistica M.G. Morgagni Forlì Italy
Introduction
Acute chest syndrome (ACS) is the leading cause of death in people with sickle cell disease (SCD ) and is a major cause of morbidity [1, 2] since about 50% of patients with SCD experience at least one episode of ACS in their life. ACS is defined by the appearance of new pulmonary infiltrates on chest X-rays accompanied by symptoms as fever, cough and chest pain. Several processes have been recognized to be related with ACS as pulmonary fat embolism, infections and vaso-occlusive events.
Case history
A 22-years-male with an history of double etherozigosis sickle cell disease and beta talassemia presented with septic fever since few days, thoracic pain and dyspnea. The patients showed at the physical examination high respiratory frequency and bilateral crackles at auscultation. The ABG was: pH 7.46, pa O2 56 mmHg, PCO2 26 mmHg, and the laboratory tests revealed anemia, leucocytosis (high neutrophilic count) and high levels of LDH. The chest radiograph showed bilateral pulmonary infiltrates at lower lobes (Figure 1) and HRCT confirmed bibasilar areas of alveolar opacification (Figure 2).

Figure 1 Chest radiograph at admission showing bilateral infiltrates.
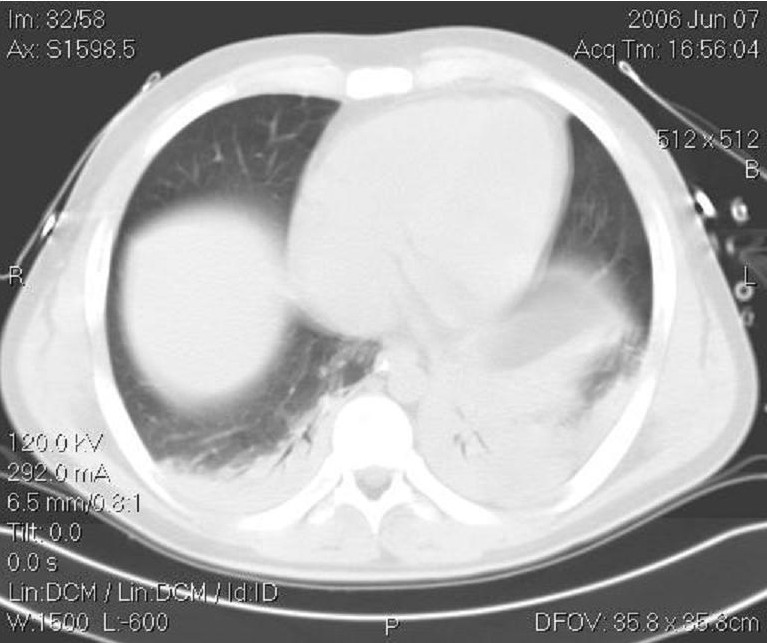
Figure 2 HRCT scan showing basal infiltrates left > right.
The patient underwent bronchoscopy and bronchoalveolar lavage (BAL) was performed. BAL fluid (BALF) was analyzed using different procedures. Diff Quick staining showed foamy marophages and cocci (Figure 3) that appeared to be Neisseria Meningitidis at microbiological culture (Figure 4). The staining “Oil Red –O” -specific for mineral oils and lipids- depicted the optically empty vacuoles (Figure 5).
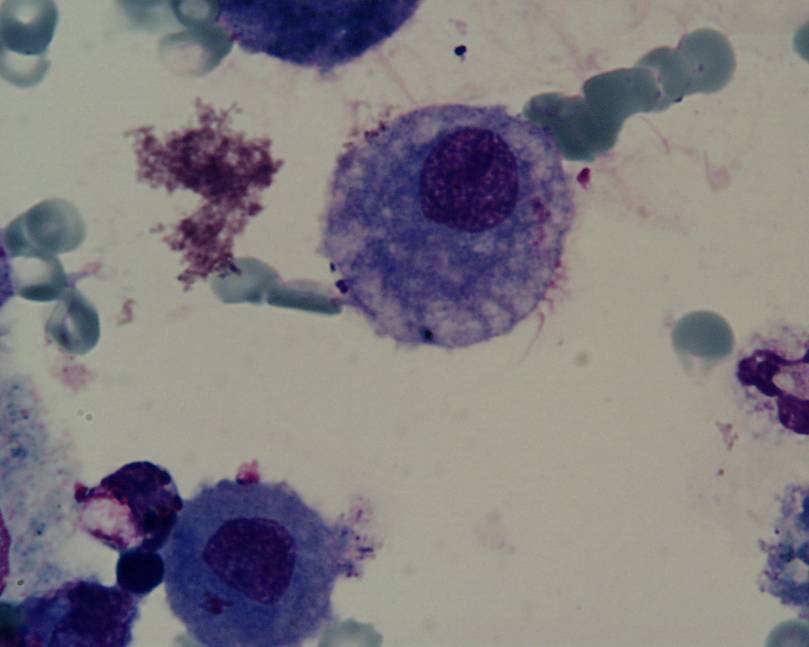
Figure 3 GIEMSA staining of BALF: foamy macrophages and cocci.
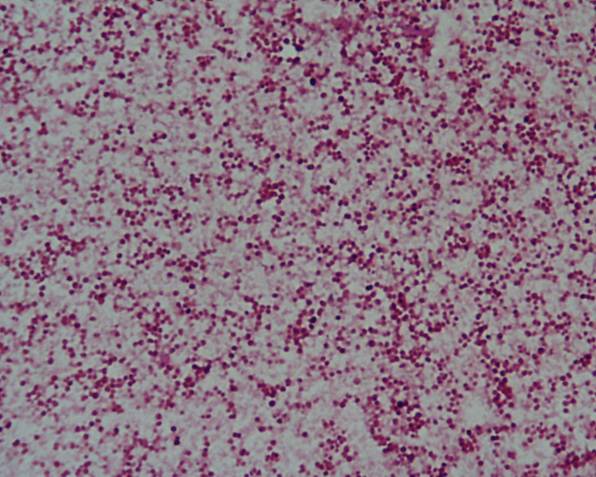
Figure 4 Culture from BALF :growth of Neisseria Meningitidis cocci.
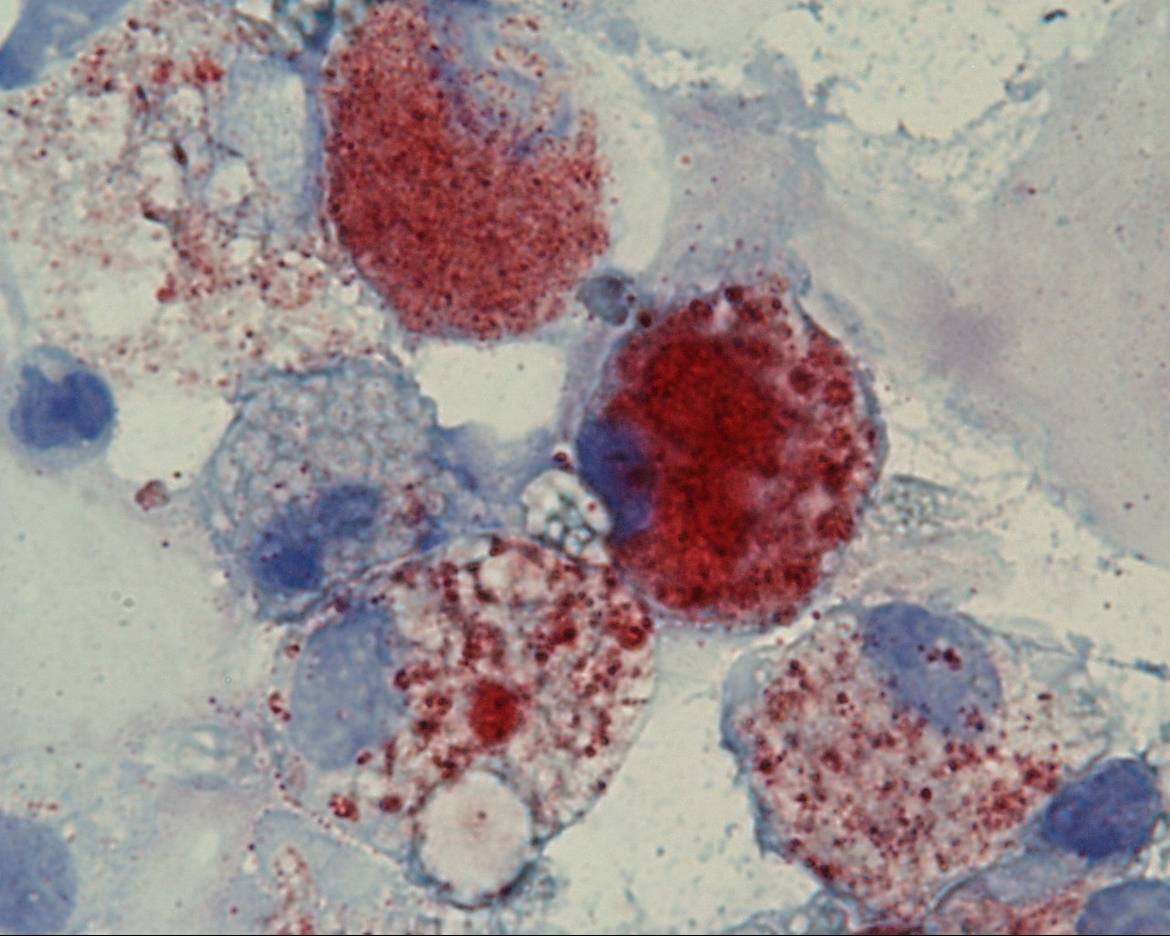
Figure 5 ORO staining of BAL fluid : lipid laden macrophages.
The patient was treated with proper antibiotic therapy on the basis of microbiologic culture and with steroids, supplemental oxygen, and iv rehydration.
Discussion ACS has a great impact on people affected by sickle cell anemia: 50% of patients experience at least one episode of ACS in their life; older patients have more severe episodes [3]. Pulmonary fat embolism from bone marrow infarction and infections are frequent cause of ACS [1]. BAL hallmarks in ACS are: presence of macrophages containing optically empty vacuoles in their cytoplasm and –not constantly- presence of bacteria. Optically empty vacuoles are well stained with specific products identifying lipids. Microbiological investigations are useful to better define the nature of microorganisms. FBS is an useful tool in the suspect of acute chest syndrome since analysis of BAL fluid may be useful for a precise clinical work-up in patients with this syndrome.
References
- Vichinsky EP, Neumayr LD, Earles AN et al Causes and outcome of acute chest syndrome in sickle cell disease New Engl J Med 2000; 342: 1856-65.
- Minter KR, Gladwin MT Pulmonary complication of sickle cell anemia. Am J Resp Crit Care Med 2001; 164: 2016-19.
- Vichinsky EP, Styles LA, Colangelo LH et al Acute chest syndrome ein sickle cell disease: clinical presentation and course Blood 1997; 89:1787-92.
Feedback & comments
If you would like to share any comments on this case please send them to wasog@gosker.nl and after peer review your comment(s) will be posted below.